Distal Biceps Tear
April 23, 2018
Sports Medicine Review – Dermatology Review
April 24, 2018Lateral Epicondylitis

Lateral Epicondylitis
Description
Lateral Epicondylitis occurs in ~1-3% of adults and is more commonly referred to as “Tennis Elbow”.1 It is an injury caused by repetitive use that results in degeneration at the origin of the extensor tendons.1,3 The forearm extensor muscles include: extensor carpi radialis brevis, extensor digitorum, extensor Digiti minimi, and extensor carpi ulnaris.2 The ECRB is most often involved. 1,2,3
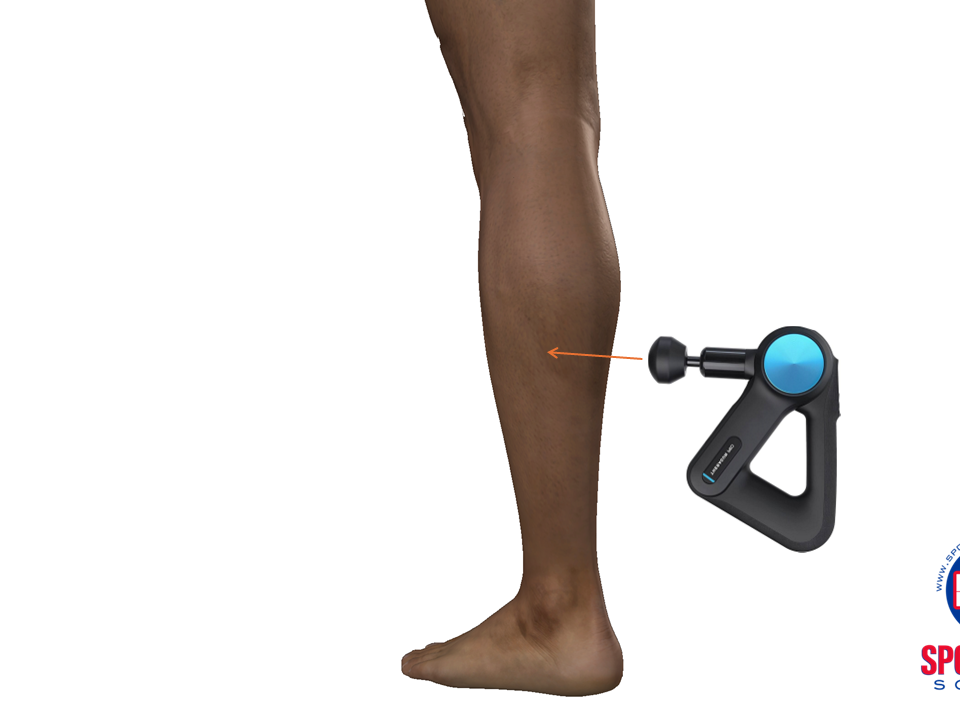
Figure 1 – Anatomy of Lateral Epicondyle
![]()
Although it is referred to as epicondylitis the term “tendinosis” has been preferred due the chronic degenerative nature of this condition 1,2. Patients will describe insidious onset and gradual progression of pain and weakness. The pain is at the lateral aspect of the elbow. 1,2 It often radiates down the forearm. They may endorse weakness in grip strength that affects their sport or work activities. 1
Injury mechanism:
Microtrauma from repetitive wrist extension and alternating forearm supination and pronation. 1,2
There is an acute inflammatory response, followed by angiofibroblastic hyperplasia and finally fibrosis if there is prolonged and sustained insult. 2,1
Although associated with tennis, this type of injury can be seen in anyone who repetitively extend and supinate their forearms. 2,3 This includes activities such as racquet sports, prolonged computer sitting, piano playing, and manual work. 1,2
Differential Diagnosis:1,2
- Cervical Radiculopathy
- Entrapment of Posterior Interosseous Nerve (Radial Tunnel Syndrome)
- Lateral Ulnar Collateral Ligament insufficiency (Posterolateral rotator instability)
- Osteochondritis dissecans of capitellum
- Radial head fracture
- Radiocapitellar osteoarthritis
- Elbow Plica
- Inflammatory or Degenerative Arthritis (e.g. Rheumatoid Arthritis or Osteoarthritis)
- Infection
Physical Exam:
Tenderness at lateral epicondyle and along extensor muscular mass distal to epicondyle. 1
Worsened with passive wrist flexion and resisted active wrist extension with the elbow extended. 1,2
It is important to examine the elbow for ulnar collateral ligament insufficiency and the shoulder as patients may be compensating for a shoulder injury. 1
Investigations:
Imaging is not necessary for initial treatment but may help to rule out other causes of pain (arthritis, osteochondritis dissecans). 2,3
X-ray: Calcifications in soft tissue at or near insertion of the ECRB on the lateral epicondyle. 1
Ultrasound: Identify thickening, hypoechogenic foci, tendon tears, calcification, or boney deposits in the affected tendons. 2
MRI: More reproducible form of imaging which reduces intra-operator variability. 2,3 MRI imaging may confirm the diagnosis, and show degenerative tissues and tears, intra-articular loose bodies, and osteochondral defects. 1,2 Studies have shown MRI has 90-100% sensitivity and 83-100% specificity for detecting epicondylitis. 1
EMG can help exclude posterior interosseous nerve entrapment.
Management:
First line treatment is non-surgical conservative management. This includes rest, NSAIDs, bracing, and physical therapy. 1 Emphasis is on pain control, preservation of movement and improvement of function. 1,2 An elbow strap that applies pressure to the musculotendinous junction of the extensors may reduce pain for activities of daily living.
Physical therapy includes strengthening and stretching the extensor muscles. 1,2 This can include eccentric exercises. 2
In patients who do not improve with initial treatment alternative therapies such as glucocorticoid injections, acupuncture, botulin injection, platelet rich plasma injections, and shockwave therapy may be explored. 1 There are well over 10 treatments described for this condition including a comparison trial between topical diclofenac and leeches. The number of treatments speaks to the frequency of failure of treatments as well as the duration of symptoms.
Although most respond to initial treatment some will require surgical management. 1,4
Surgical treatment is reserved for those who have not responded to non-operative therapy for at least 6 months or in those who continue to have marked dysfunction. 1,2,4 The procedure involves resection of tendinosis tissue with or without repair of the extensor carpi radialis brevis. 1,2 This may be done via open or arthroscopic technique. 1,2,4
Return to Sport
Patients return to sport varies depending on the extent of the injury and the athlete. They may return to sport as long as they are able to avoid aggravating activities. This can include playing in a modified way and improving mechanics of improper technique. 1,4
Author Dr. Sumeet Gill (April 21, 2018 PR ND)
References:
1) Brummel, J., Champ, L., Baker III, Hopkins, R., & Champ L.B., (2014). Epicondylitis: Lateral. (2014). Sport Med Arthroscopic Review.
2) Ahmad, Z., Siddiqui, N., Malik, S. S., Abdus-Samee, M., Tytherleigh-Strong, G., & Rushton, N. (2013). Lateral Epicondylitis: A Review of Pathology & Management. The Bone & Joint Journal.
3) Jeon, J.Y, Hee-Lee, M., Jeon, I,H., Chung, H.W., Lee, S.H., Shin, M.J. (2017). Lateral Epicondylitis: Associations of MR Imaging and clinical assessment with treatment option in patient receiving conservative and Arthroscopic managements. European Society Of Radiology.
4) Burn, M.B., Mitchell, R.J., Liberman, S.R., Lintner, D.M., Harris, J.D., McCulloch, P. (2017). Open, Arthroscopic, and Percutaneous Surgical Treatment of Lateral Epicondylitis: A Systematic Review. American Association of Hand Surgery.